Tips On How To Diagnose Fallen Arches
Overview

A normal foot should arch so the middle of the foot does not touch the ground when the patient stands up. If it does touch, the patient has a flat foot or fallen arch. Flat feet are normal for young children. Their arches should develop by adulthood, but sometimes they fail to develop. Some people with flat feet have pain in the heel or arch, but others do not.
Causes
Most cases of flatfeet are simply the result of normal development. When that is not the case, the condition can be caused by a number of factors, including the following, Age, disease, injury, obesity or being overweight, physical abnormality, pregnancy. Flattened arches in adults may result from the stresses of aging, weight gain, and the temporary increase in elastin (protein in connective tissue) due to pregnancy. In some cases, flatfeet are caused by a physical abnormality, such as tarsal coalition (two or more bones in the foot that have grown together) or accessory navicular (an extra bone along the side of the foot). The effects of diseases such as diabetes and rheumatoid arthritis can lead to flatfeet. An injury (e.g., bone fracture, dislocation, sprain or tear in any of the tendons and ligaments in the foot and leg) also can cause flatfeet.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms below. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
You can always give yourself the ?wet test? described above to see whether you have flat feet. Most people who do not notice their flat feet or have no pain associated with them do not think to see a foot doctor. Flat feet can lead to additional problems such as stiffness or pain, however, especially if the condition appears out of nowhere. If you think you may have flat feet, you should seek medical attention to ensure there are no additional issues to worry about. Your doctor will be able to diagnose you with a number of tests. For example, he or she may have you walk around, stand still, or stand on your tiptoes while you are being examined. Your doctor may also examine your foot?s shape and functionality. It?s important to let your foot doctor know about your medical and family history. In some cases, your doctor may order imaging tests such as x-rays or an MRI (magnetic resonance imaging) to determine a cause of your flat foot. If tarsal coalition is suspected in children, a CT scan is often ordered.
fallen arches surgery
Non Surgical Treatment
If you have flat feet and foot pain, especially if one foot is flatter than the other, you should have an evaluation by an orthopedic surgeon . You may have a problem with the posterior tibial tendon , the main tendon that supports the arch. Factors that can contribute to this problem are obesity, diabetes , high blood pressure , certain types of arthritis and athletic overuse. In some cases a shoe insert/orthotic can be used to alleviate the symptoms of flat feet.
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer). Flat feet and fallen arches are common conditions that are in most cases asymptomatic. However, in patients who do have symptoms, treatments are available that can help reduce pain and promote efficient movement. Orthotic devices are well recognised as an excellent treatment and podiatrists can offer these different treatment modalities as individualised treatments for patients.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.

A normal foot should arch so the middle of the foot does not touch the ground when the patient stands up. If it does touch, the patient has a flat foot or fallen arch. Flat feet are normal for young children. Their arches should develop by adulthood, but sometimes they fail to develop. Some people with flat feet have pain in the heel or arch, but others do not.
Causes
Most cases of flatfeet are simply the result of normal development. When that is not the case, the condition can be caused by a number of factors, including the following, Age, disease, injury, obesity or being overweight, physical abnormality, pregnancy. Flattened arches in adults may result from the stresses of aging, weight gain, and the temporary increase in elastin (protein in connective tissue) due to pregnancy. In some cases, flatfeet are caused by a physical abnormality, such as tarsal coalition (two or more bones in the foot that have grown together) or accessory navicular (an extra bone along the side of the foot). The effects of diseases such as diabetes and rheumatoid arthritis can lead to flatfeet. An injury (e.g., bone fracture, dislocation, sprain or tear in any of the tendons and ligaments in the foot and leg) also can cause flatfeet.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms below. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
You can always give yourself the ?wet test? described above to see whether you have flat feet. Most people who do not notice their flat feet or have no pain associated with them do not think to see a foot doctor. Flat feet can lead to additional problems such as stiffness or pain, however, especially if the condition appears out of nowhere. If you think you may have flat feet, you should seek medical attention to ensure there are no additional issues to worry about. Your doctor will be able to diagnose you with a number of tests. For example, he or she may have you walk around, stand still, or stand on your tiptoes while you are being examined. Your doctor may also examine your foot?s shape and functionality. It?s important to let your foot doctor know about your medical and family history. In some cases, your doctor may order imaging tests such as x-rays or an MRI (magnetic resonance imaging) to determine a cause of your flat foot. If tarsal coalition is suspected in children, a CT scan is often ordered.
fallen arches surgery
Non Surgical Treatment
If you have flat feet and foot pain, especially if one foot is flatter than the other, you should have an evaluation by an orthopedic surgeon . You may have a problem with the posterior tibial tendon , the main tendon that supports the arch. Factors that can contribute to this problem are obesity, diabetes , high blood pressure , certain types of arthritis and athletic overuse. In some cases a shoe insert/orthotic can be used to alleviate the symptoms of flat feet.
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer). Flat feet and fallen arches are common conditions that are in most cases asymptomatic. However, in patients who do have symptoms, treatments are available that can help reduce pain and promote efficient movement. Orthotic devices are well recognised as an excellent treatment and podiatrists can offer these different treatment modalities as individualised treatments for patients.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
What Are The Major Causes Of Heel Painfulness
Overview

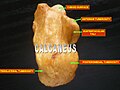
Heel pain is common and can be due to a number of conditions. The calcaneus (heel bone) is the largest bone in the foot and is the first to hit the ground when walking. The heel bone is designed to be the first contact the foot has with the ground. The achilles tendon inserts into the back of the heel bone (calcaneus) and a very strong ligament along the bottom of the foot attaches to the bottom of the heel bone (the plantar fascia). Several small muscles also attach to the heel bone above the insertion of the plantar fascia. Given the forces of walking that the heel bone is subjected to and the pull of all these ligaments and muscles, then it is not surprising that heel pain is so common.
Causes
Near the inflamed plantar fascia attachment, but not in it, some extra bone may form, producing a small "spur". In fact, it is a shelf of bone, not a sharp spur. These "heel spurs" are commoner in people with plantar fascitis, but they can be found in people with no heel pain. The heel spur is caused by the same process as the heel pain, but the spur is not itself the cause of the pain.
Symptoms
Usually when a patient comes in they?ll explain that they have severe pain in the heel. It?s usually worse during the first step in the morning when they get out of bed. Many people say if they walk for a period of time, it gets a little bit better. But if they sit down and get back up, the pain will come back and it?s one of those intermittent come and go types of pain. Heel pain patients will say it feels like a toothache in the heel area or even into the arch area. A lot of times it will get better with rest and then it will just come right back. So it?s one of those nuisance type things that just never goes away. The following are common signs of heel pain and plantar fasciitis. Pain that is worse first thing in the morning. Pain that develops after heavy activity or exercise. Pain that occurs when standing up after sitting for a long period of time. Severe, toothache type of pain in the bottom of the heel.
Diagnosis
The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders.
Non Surgical Treatment
If you have experienced painful heels try wearing your shoes around your house in the evening. Don't wear slippers or socks or go barefoot. You may also try gentle calf stretches for 20 to 30 seconds on each leg. This is best done barefoot, leaning forward towards a wall with one foot forward and one foot back. If the pain persists longer than one month, you should visit a podiatrist for evaluation and treatment. Your feet should not hurt, and professional podiatric care may be required to help relieve your discomfort. If you have not exercised in a long time, consult your podiatric physician before starting a new exercise program. Begin an exercise program slowly. Don't go too far or too fast. Purchase and maintain good shoes and replace them regularly. Stretch each foot and achilles tendon before and after exercise. Avoid uneven walking surfaces or stepping on rocks as much as possible. Avoid going barefoot on hard surfaces. Vary the incline on a treadmill during exercise. Nobody walks uphill all the time. If it hurts, stop. Don't try to "work through the pain." Your podiatric physician/surgeon has been trained specifically and extensively in the diagnosis and treatment of all manner of foot conditions. This training encompasses all of the intricately related systems and structures of the foot and lower leg including neurological, circulatory, skin, and the musculoskeletal system, which includes bones, joints, ligaments, tendons, muscles, and nerves.
Surgical Treatment
Only a relatively few cases of heel pain require surgery. If required, surgery is usually for the removal of a spur, but also may involve release of the plantar fascia, removal of a bursa, or a removal of a neuroma or other soft-tissue growth.
replacement ankle straps for heels
Prevention

Make sure you wear appropriate supportive shoes. Don't over-train in sports. Make sure you warm up, cool down and undertake an exercise regime that helps maintain flexibility. Manage your weight, obesity is a factor in causing plantar fasciitis. Avoid walking and running on hard surfaces if you are prone to pain. You should follow the recognized management protocol "RICED" rest, ice, compression, elevation and diagnosis. Rest, keep off the injured ankle as much as possible. Ice, applied for 20 minutes at a time every hour as long as swelling persists. Compression, support the ankle and foot with a firmly (not tightly) wrapped elastic bandage. Elevation, keep foot above heart level to minimize bruising and swelling. Diagnosis. Consult a medical professional (such as a Podiatrist or doctor) especially if you are worried about the injury, or if the pain or swelling gets worse. If the pain or swelling has not gone down significantly within 48 hours, also seek treatment. An accurate diagnosis is essential for proper rehabilitation of moderate to severe injuries.

Heel pain is common and can be due to a number of conditions. The calcaneus (heel bone) is the largest bone in the foot and is the first to hit the ground when walking. The heel bone is designed to be the first contact the foot has with the ground. The achilles tendon inserts into the back of the heel bone (calcaneus) and a very strong ligament along the bottom of the foot attaches to the bottom of the heel bone (the plantar fascia). Several small muscles also attach to the heel bone above the insertion of the plantar fascia. Given the forces of walking that the heel bone is subjected to and the pull of all these ligaments and muscles, then it is not surprising that heel pain is so common.
Causes
Near the inflamed plantar fascia attachment, but not in it, some extra bone may form, producing a small "spur". In fact, it is a shelf of bone, not a sharp spur. These "heel spurs" are commoner in people with plantar fascitis, but they can be found in people with no heel pain. The heel spur is caused by the same process as the heel pain, but the spur is not itself the cause of the pain.
Symptoms
Usually when a patient comes in they?ll explain that they have severe pain in the heel. It?s usually worse during the first step in the morning when they get out of bed. Many people say if they walk for a period of time, it gets a little bit better. But if they sit down and get back up, the pain will come back and it?s one of those intermittent come and go types of pain. Heel pain patients will say it feels like a toothache in the heel area or even into the arch area. A lot of times it will get better with rest and then it will just come right back. So it?s one of those nuisance type things that just never goes away. The following are common signs of heel pain and plantar fasciitis. Pain that is worse first thing in the morning. Pain that develops after heavy activity or exercise. Pain that occurs when standing up after sitting for a long period of time. Severe, toothache type of pain in the bottom of the heel.
Diagnosis
The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders.
Non Surgical Treatment
If you have experienced painful heels try wearing your shoes around your house in the evening. Don't wear slippers or socks or go barefoot. You may also try gentle calf stretches for 20 to 30 seconds on each leg. This is best done barefoot, leaning forward towards a wall with one foot forward and one foot back. If the pain persists longer than one month, you should visit a podiatrist for evaluation and treatment. Your feet should not hurt, and professional podiatric care may be required to help relieve your discomfort. If you have not exercised in a long time, consult your podiatric physician before starting a new exercise program. Begin an exercise program slowly. Don't go too far or too fast. Purchase and maintain good shoes and replace them regularly. Stretch each foot and achilles tendon before and after exercise. Avoid uneven walking surfaces or stepping on rocks as much as possible. Avoid going barefoot on hard surfaces. Vary the incline on a treadmill during exercise. Nobody walks uphill all the time. If it hurts, stop. Don't try to "work through the pain." Your podiatric physician/surgeon has been trained specifically and extensively in the diagnosis and treatment of all manner of foot conditions. This training encompasses all of the intricately related systems and structures of the foot and lower leg including neurological, circulatory, skin, and the musculoskeletal system, which includes bones, joints, ligaments, tendons, muscles, and nerves.
Surgical Treatment
Only a relatively few cases of heel pain require surgery. If required, surgery is usually for the removal of a spur, but also may involve release of the plantar fascia, removal of a bursa, or a removal of a neuroma or other soft-tissue growth.
replacement ankle straps for heels
Prevention

Make sure you wear appropriate supportive shoes. Don't over-train in sports. Make sure you warm up, cool down and undertake an exercise regime that helps maintain flexibility. Manage your weight, obesity is a factor in causing plantar fasciitis. Avoid walking and running on hard surfaces if you are prone to pain. You should follow the recognized management protocol "RICED" rest, ice, compression, elevation and diagnosis. Rest, keep off the injured ankle as much as possible. Ice, applied for 20 minutes at a time every hour as long as swelling persists. Compression, support the ankle and foot with a firmly (not tightly) wrapped elastic bandage. Elevation, keep foot above heart level to minimize bruising and swelling. Diagnosis. Consult a medical professional (such as a Podiatrist or doctor) especially if you are worried about the injury, or if the pain or swelling gets worse. If the pain or swelling has not gone down significantly within 48 hours, also seek treatment. An accurate diagnosis is essential for proper rehabilitation of moderate to severe injuries.
Leg Length Discrepancy Lifts
Overview
Differences of an inch-and-a-half to two inches may require epiphysiodesis (adjusting the growth of the longer side) or acute shortening of the other side. Differences greater than 2.5 inches usually require a lengthening procedure. The short bone is cut and an external device is applied. Gradual lengthening is done over months to allow the muscles and nerves accommodate the new length.
Causes
The causes of LLD are many, including a previous injury, bone infection, bone diseases (dysplasias), inflammation (arthritis) and neurologic conditions. Previously broken bones may cause LLD by healing in a shortened position, especially if the bone was broken in many pieces (comminuted) or if skin and muscle tissue around the bone were severely injured and exposed (open fracture). Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. Also, a break in a child?s bone through a growth center (located near the ends of the bone) may cause slower growth, resulting in a shorter extremity. Bone infections that occur in children while they are growing may cause a significant LLD, especially during infancy. Bone diseases may cause LLD, as well; examples are neurofibromatosis, multiple hereditary exostoses and Ollier disease. Inflammation of joints during growth may cause unequal extremity length. One example is juvenile rheumatoid arthritis. Osteoarthritis, the joint degeneration that occurs in adults, very rarely causes a significant LLD.
Symptoms
Children whose limbs vary in length often experience difficulty using their arms or legs. They might have difficulty walking or using both arms to engage in everyday activities.
Diagnosis
A doctor will generally take a detailed medical history of both the patient and family, including asking about recent injuries or illnesses. He or she will carefully examine the patient, observing how he or she moves and stands. If necessary, an orthopedic surgeon will order X-ray, bone age determinations and computed tomography (CT) scans or magnetic resonance imaging (MRI).
Non Surgical Treatment
The non-surgical intervention is mainly usedfor the functional and environmental types of leg length discrepancies. It is also applied to the mild category of limb length inequality. Non-surgical intervention consists of stretching the muscles of the lower extremity. This is individually different, whereby the M. Tensor Fascia latae, the adductors, the hamstring muscles, M. piriformis and M. Iliopsoas are stretched. In this non-surgical intervention belongs also the use of shoe lifts. These shoe lifts consists of either a shoe insert (up to 10-20mm of correction), or building up the sole of the shoe on the shorter leg (up to 30-60mm of correction). This lift therapy should be implemented gradually in small increments. Several studies have examined the treatment of low back pain patients with LLD with shoe lifts. Gofton obtained good results: the patients experienced major or complete pain relief that lasted upon follow-up ranging from 3 to 11 years. Helliwell also observed patients whereby 44% experienced complete pain relief, and 45% had moderate or substantial pain relief. Friberg found that 157 (of 211) patients with LBP, treated with shoe lifts, were symprom-free after a mean follow-up of 18 months.

functional leg length discrepancy treatment
Surgical Treatment
In growing children, legs can be made equal or nearly equal in length with a relatively simple surgical procedure. This procedure slows down the growth of the longer leg at one or two growth sites. Your physician can tell you how much equalization can be gained by this procedure. The procedure is performed under X-ray control through very small incisions in the knee area. This procedure will not cause an immediate correction in length. Instead, the limb length discrepancy will gradually decrease as the opposite extremity continues to grow and "catch up." Timing of the procedure is critical. The goal is to reach equal leg length by the time growth normally ends. This is usually in the mid-to-late teenage years. Disadvantages of this option include the possibility of slight over-correction or under-correction of the limb length discrepancy. In addition, the patient's adult height will be less than if the shorter leg had been lengthened. Correction of significant limb length discrepancy by this method may make a patient's body look slightly disproportionate because of the shorter leg. In some cases the longer leg can be shortened, but a major shortening may weaken the muscles of the leg. In the thighbone (femur), a maximum of 3 inches can be shortened. In the shinbone, a maximum of 2 inches can be shortened.
Differences of an inch-and-a-half to two inches may require epiphysiodesis (adjusting the growth of the longer side) or acute shortening of the other side. Differences greater than 2.5 inches usually require a lengthening procedure. The short bone is cut and an external device is applied. Gradual lengthening is done over months to allow the muscles and nerves accommodate the new length.

Causes
The causes of LLD are many, including a previous injury, bone infection, bone diseases (dysplasias), inflammation (arthritis) and neurologic conditions. Previously broken bones may cause LLD by healing in a shortened position, especially if the bone was broken in many pieces (comminuted) or if skin and muscle tissue around the bone were severely injured and exposed (open fracture). Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. Also, a break in a child?s bone through a growth center (located near the ends of the bone) may cause slower growth, resulting in a shorter extremity. Bone infections that occur in children while they are growing may cause a significant LLD, especially during infancy. Bone diseases may cause LLD, as well; examples are neurofibromatosis, multiple hereditary exostoses and Ollier disease. Inflammation of joints during growth may cause unequal extremity length. One example is juvenile rheumatoid arthritis. Osteoarthritis, the joint degeneration that occurs in adults, very rarely causes a significant LLD.
Symptoms
Children whose limbs vary in length often experience difficulty using their arms or legs. They might have difficulty walking or using both arms to engage in everyday activities.
Diagnosis
A doctor will generally take a detailed medical history of both the patient and family, including asking about recent injuries or illnesses. He or she will carefully examine the patient, observing how he or she moves and stands. If necessary, an orthopedic surgeon will order X-ray, bone age determinations and computed tomography (CT) scans or magnetic resonance imaging (MRI).
Non Surgical Treatment
The non-surgical intervention is mainly usedfor the functional and environmental types of leg length discrepancies. It is also applied to the mild category of limb length inequality. Non-surgical intervention consists of stretching the muscles of the lower extremity. This is individually different, whereby the M. Tensor Fascia latae, the adductors, the hamstring muscles, M. piriformis and M. Iliopsoas are stretched. In this non-surgical intervention belongs also the use of shoe lifts. These shoe lifts consists of either a shoe insert (up to 10-20mm of correction), or building up the sole of the shoe on the shorter leg (up to 30-60mm of correction). This lift therapy should be implemented gradually in small increments. Several studies have examined the treatment of low back pain patients with LLD with shoe lifts. Gofton obtained good results: the patients experienced major or complete pain relief that lasted upon follow-up ranging from 3 to 11 years. Helliwell also observed patients whereby 44% experienced complete pain relief, and 45% had moderate or substantial pain relief. Friberg found that 157 (of 211) patients with LBP, treated with shoe lifts, were symprom-free after a mean follow-up of 18 months.

functional leg length discrepancy treatment
Surgical Treatment
In growing children, legs can be made equal or nearly equal in length with a relatively simple surgical procedure. This procedure slows down the growth of the longer leg at one or two growth sites. Your physician can tell you how much equalization can be gained by this procedure. The procedure is performed under X-ray control through very small incisions in the knee area. This procedure will not cause an immediate correction in length. Instead, the limb length discrepancy will gradually decrease as the opposite extremity continues to grow and "catch up." Timing of the procedure is critical. The goal is to reach equal leg length by the time growth normally ends. This is usually in the mid-to-late teenage years. Disadvantages of this option include the possibility of slight over-correction or under-correction of the limb length discrepancy. In addition, the patient's adult height will be less than if the shorter leg had been lengthened. Correction of significant limb length discrepancy by this method may make a patient's body look slightly disproportionate because of the shorter leg. In some cases the longer leg can be shortened, but a major shortening may weaken the muscles of the leg. In the thighbone (femur), a maximum of 3 inches can be shortened. In the shinbone, a maximum of 2 inches can be shortened.
Mortons Neuroma Cures
Overview
 Morton's Neuroma is a common problem in runners, and there are a number of simple fixes you can try before resorting more drastic solutions like sclerosing or surgery. A Morton's Neuroma normally causes a burning pain in the forefoot, just behind the 3rd and 4th toes (sometimes behind the 2nd and 3rd toes). The pain often radiates towards the toes, and sometimes there is numbness rather than pain. The underlying cause is inflammation of the nerve between the bones of the forefoot, often triggered by narrow or tight shoes. I have had good results with the simple fixes described below, and I have had reports of other runners with similar success.
Morton's Neuroma is a common problem in runners, and there are a number of simple fixes you can try before resorting more drastic solutions like sclerosing or surgery. A Morton's Neuroma normally causes a burning pain in the forefoot, just behind the 3rd and 4th toes (sometimes behind the 2nd and 3rd toes). The pain often radiates towards the toes, and sometimes there is numbness rather than pain. The underlying cause is inflammation of the nerve between the bones of the forefoot, often triggered by narrow or tight shoes. I have had good results with the simple fixes described below, and I have had reports of other runners with similar success.
Causes
Anything that causes compression or irritation of the nerve can lead to the development of a neuroma. One of the most common causes comes from wearing shoes that have a tapered toe box, or high-heeled shoes that cause the toes to be forced into the toe box and overload pressure onto the forefoot. An injury or trauma to the forefoot may also lead to a neuroma. People at a higher risk of developing a Neuroma include people with certain foot deformities, such as bunions or hammertoes. Certain foot types, such as flat feet (Pronation) More flexible feet, and woman after pregnancy.
Symptoms
Typically, there's no outward sign of this condition, such as a lump. Instead, you may experience the following symptoms. A feeling as if you're standing on a pebble in your shoe. A burning pain in the ball of your foot that may radiate into your toes. Tingling or numbness in your toes. It's best not to ignore any foot pain that lasts longer than a few days. See your doctor if you experience a burning pain in the ball of your foot that's not improving, despite changing your footwear and modifying activities that may cause stress to your foot.
Diagnosis
Patients with classic Morton?s neuroma symptoms will have pain with pressure at the base of the involved toes (either between the 2nd and 3rd toes, or between the 3rd and 4th toes). In addition, squeezing the front of the foot together can exacerbate symptoms. As well, they may have numbness on the sides of one toe and the adjacent toe as this corresponds with the distribution of the involved nerve.
Non Surgical Treatment
Treatment options vary with the severity of each neuroma, and identifying the neuroma early in its development is important to avoid surgical correction. For simple, undeveloped neuromas, a pair of thick-soled shoes with a wide toe box is often adequate treatment to relieve symptoms, allowing the condition to diminish on its own. For more severe conditions, however, additional treatment or surgery may be necessary to remove the tumor. The primary goal of most early treatment regimens is to relieve pressure on areas where a neuroma develops. Your podiatric physician will examine and likely X-ray the affected area and suggest a treatment plan that best suits your individual case. Padding and Taping. Special padding at the ball of the foot may change the abnormal foot function and relieve the symptoms caused by the neuroma. Medication. Anti-inflammatory drugs and cortisone injections can be prescribed to ease acute pain and inflammation caused by the neuroma. Orthotics. Custom shoe inserts made by your podiatrist may be useful in controlling foot function. Orthotics may reduce symptoms and prevent the worsening of the condition.
Surgical Treatment
If your pain continues despite several months of conservative treatment, your doctor may recommend surgery to remove the neuroma or to widen the space through which the affected nerve travels. These types of surgery often are done under local anesthesia. If your doctor removes a portion of the affected nerve along with the neuroma, you may develop permanent numbness between the toes.
Prevention
The best way to prevent a neuroma is by avoiding the things that cause them. Review your risk factors. If relatives have had similar problems, or if you know that you pronate or have any problem with the mechanics of your foot, talk with a podiatric physician about the correct types of shoes and/or orthoses for you. If you are not sure whether you have such a problem, the podiatric professional can analyze your foot, your stride and the wear pattern of your shoes, and give you an honest evaluation. Remember, though, that sometimes neuromas, like other conditions, can develop for no discernible reason. With this in mind, be good to your feet, and be aware of any changes or problems. Don?t wait to report them.
 Morton's Neuroma is a common problem in runners, and there are a number of simple fixes you can try before resorting more drastic solutions like sclerosing or surgery. A Morton's Neuroma normally causes a burning pain in the forefoot, just behind the 3rd and 4th toes (sometimes behind the 2nd and 3rd toes). The pain often radiates towards the toes, and sometimes there is numbness rather than pain. The underlying cause is inflammation of the nerve between the bones of the forefoot, often triggered by narrow or tight shoes. I have had good results with the simple fixes described below, and I have had reports of other runners with similar success.
Morton's Neuroma is a common problem in runners, and there are a number of simple fixes you can try before resorting more drastic solutions like sclerosing or surgery. A Morton's Neuroma normally causes a burning pain in the forefoot, just behind the 3rd and 4th toes (sometimes behind the 2nd and 3rd toes). The pain often radiates towards the toes, and sometimes there is numbness rather than pain. The underlying cause is inflammation of the nerve between the bones of the forefoot, often triggered by narrow or tight shoes. I have had good results with the simple fixes described below, and I have had reports of other runners with similar success.Causes
Anything that causes compression or irritation of the nerve can lead to the development of a neuroma. One of the most common causes comes from wearing shoes that have a tapered toe box, or high-heeled shoes that cause the toes to be forced into the toe box and overload pressure onto the forefoot. An injury or trauma to the forefoot may also lead to a neuroma. People at a higher risk of developing a Neuroma include people with certain foot deformities, such as bunions or hammertoes. Certain foot types, such as flat feet (Pronation) More flexible feet, and woman after pregnancy.
Symptoms
Typically, there's no outward sign of this condition, such as a lump. Instead, you may experience the following symptoms. A feeling as if you're standing on a pebble in your shoe. A burning pain in the ball of your foot that may radiate into your toes. Tingling or numbness in your toes. It's best not to ignore any foot pain that lasts longer than a few days. See your doctor if you experience a burning pain in the ball of your foot that's not improving, despite changing your footwear and modifying activities that may cause stress to your foot.
Diagnosis
Patients with classic Morton?s neuroma symptoms will have pain with pressure at the base of the involved toes (either between the 2nd and 3rd toes, or between the 3rd and 4th toes). In addition, squeezing the front of the foot together can exacerbate symptoms. As well, they may have numbness on the sides of one toe and the adjacent toe as this corresponds with the distribution of the involved nerve.
Non Surgical Treatment
Treatment options vary with the severity of each neuroma, and identifying the neuroma early in its development is important to avoid surgical correction. For simple, undeveloped neuromas, a pair of thick-soled shoes with a wide toe box is often adequate treatment to relieve symptoms, allowing the condition to diminish on its own. For more severe conditions, however, additional treatment or surgery may be necessary to remove the tumor. The primary goal of most early treatment regimens is to relieve pressure on areas where a neuroma develops. Your podiatric physician will examine and likely X-ray the affected area and suggest a treatment plan that best suits your individual case. Padding and Taping. Special padding at the ball of the foot may change the abnormal foot function and relieve the symptoms caused by the neuroma. Medication. Anti-inflammatory drugs and cortisone injections can be prescribed to ease acute pain and inflammation caused by the neuroma. Orthotics. Custom shoe inserts made by your podiatrist may be useful in controlling foot function. Orthotics may reduce symptoms and prevent the worsening of the condition.

Surgical Treatment
If your pain continues despite several months of conservative treatment, your doctor may recommend surgery to remove the neuroma or to widen the space through which the affected nerve travels. These types of surgery often are done under local anesthesia. If your doctor removes a portion of the affected nerve along with the neuroma, you may develop permanent numbness between the toes.
Prevention
The best way to prevent a neuroma is by avoiding the things that cause them. Review your risk factors. If relatives have had similar problems, or if you know that you pronate or have any problem with the mechanics of your foot, talk with a podiatric physician about the correct types of shoes and/or orthoses for you. If you are not sure whether you have such a problem, the podiatric professional can analyze your foot, your stride and the wear pattern of your shoes, and give you an honest evaluation. Remember, though, that sometimes neuromas, like other conditions, can develop for no discernible reason. With this in mind, be good to your feet, and be aware of any changes or problems. Don?t wait to report them.
Alleviating Leg Length Discrepancy With Shoe Lifts
There are not one but two different kinds of leg length discrepancies, congenital and acquired. Congenital indicates that you are born with it. One leg is structurally shorter in comparison to the other. As a result of developmental periods of aging, the brain picks up on the stride pattern and identifies some difference. The body typically adapts by tilting one shoulder to the "short" side. A difference of under a quarter inch isn't blatantly irregular, require Shoe Lifts to compensate and typically doesn't have a profound effect over a lifetime.

Leg length inequality goes largely undiscovered on a daily basis, however this issue is very easily corrected, and can eliminate quite a few instances of lower back pain.
Therapy for leg length inequality commonly involves Shoe Lifts. Many are low-priced, regularly priced at below twenty dollars, compared to a custom orthotic of $200 or maybe more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Back ache is easily the most common condition impacting people today. Over 80 million people suffer from back pain at some stage in their life. It's a problem which costs businesses vast amounts of money each year as a result of time lost and production. New and improved treatment methods are continually sought after in the hope of minimizing the economic influence this condition causes.

People from all corners of the world suffer the pain of foot ache due to leg length discrepancy. In these types of cases Shoe Lifts can be of very useful. The lifts are capable of reducing any discomfort in the feet. Shoe Lifts are recommended by countless expert orthopaedic doctors.
So that they can support the body in a balanced manner, the feet have a very important role to play. Irrespective of that, it can be the most neglected region of the body. Some people have flat-feet meaning there is unequal force placed on the feet. This will cause other body parts like knees, ankles and backs to be impacted too. Shoe Lifts guarantee that appropriate posture and balance are restored.

Leg length inequality goes largely undiscovered on a daily basis, however this issue is very easily corrected, and can eliminate quite a few instances of lower back pain.
Therapy for leg length inequality commonly involves Shoe Lifts. Many are low-priced, regularly priced at below twenty dollars, compared to a custom orthotic of $200 or maybe more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Back ache is easily the most common condition impacting people today. Over 80 million people suffer from back pain at some stage in their life. It's a problem which costs businesses vast amounts of money each year as a result of time lost and production. New and improved treatment methods are continually sought after in the hope of minimizing the economic influence this condition causes.

People from all corners of the world suffer the pain of foot ache due to leg length discrepancy. In these types of cases Shoe Lifts can be of very useful. The lifts are capable of reducing any discomfort in the feet. Shoe Lifts are recommended by countless expert orthopaedic doctors.
So that they can support the body in a balanced manner, the feet have a very important role to play. Irrespective of that, it can be the most neglected region of the body. Some people have flat-feet meaning there is unequal force placed on the feet. This will cause other body parts like knees, ankles and backs to be impacted too. Shoe Lifts guarantee that appropriate posture and balance are restored.
Shoe Lifts The Podiatrists Answer For Leg Length Discrepancy
There are actually two unique variations of leg length discrepancies, congenital and acquired. Congenital indicates you are born with it. One leg is structurally shorter compared to the other. As a result of developmental periods of aging, the human brain senses the stride pattern and recognizes some difference. The human body typically adapts by tilting one shoulder to the "short" side. A difference of under a quarter inch is not really excessive, demand Shoe Lifts to compensate and generally does not have a profound effect over a lifetime.

Leg length inequality goes mainly undiscovered on a daily basis, however this issue is very easily corrected, and can eradicate numerous instances of lower back pain.
Treatment for leg length inequality usually involves Shoe Lifts. These are very inexpensive, often being below twenty dollars, in comparison to a custom orthotic of $200 if not more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Chronic back pain is the most prevalent health problem impacting men and women today. Around 80 million men and women are affected by back pain at some point in their life. It's a problem that costs companies millions yearly because of lost time and productivity. Fresh and superior treatment solutions are always sought after in the hope of decreasing the economical impact this issue causes.

People from all corners of the earth suffer the pain of foot ache as a result of leg length discrepancy. In these cases Shoe Lifts are usually of beneficial. The lifts are capable of reducing any discomfort in the feet. Shoe Lifts are recommended by numerous certified orthopaedic doctors.
In order to support the human body in a balanced fashion, your feet have a very important part to play. Inspite of that, it is sometimes the most overlooked region of the human body. Some people have flat-feet which means there is unequal force exerted on the feet. This causes other body parts like knees, ankles and backs to be affected too. Shoe Lifts guarantee that ideal posture and balance are restored.

Leg length inequality goes mainly undiscovered on a daily basis, however this issue is very easily corrected, and can eradicate numerous instances of lower back pain.
Treatment for leg length inequality usually involves Shoe Lifts. These are very inexpensive, often being below twenty dollars, in comparison to a custom orthotic of $200 if not more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Chronic back pain is the most prevalent health problem impacting men and women today. Around 80 million men and women are affected by back pain at some point in their life. It's a problem that costs companies millions yearly because of lost time and productivity. Fresh and superior treatment solutions are always sought after in the hope of decreasing the economical impact this issue causes.

People from all corners of the earth suffer the pain of foot ache as a result of leg length discrepancy. In these cases Shoe Lifts are usually of beneficial. The lifts are capable of reducing any discomfort in the feet. Shoe Lifts are recommended by numerous certified orthopaedic doctors.
In order to support the human body in a balanced fashion, your feet have a very important part to play. Inspite of that, it is sometimes the most overlooked region of the human body. Some people have flat-feet which means there is unequal force exerted on the feet. This causes other body parts like knees, ankles and backs to be affected too. Shoe Lifts guarantee that ideal posture and balance are restored.
Have I Got Inferior Calcaneal Spur
Overview
The calcaneus is the largest bone in the foot. Pain in the heel region can sometimes be related to Plantar Fasciitis, inflammation of the plantar fascia ligament in the heel area. A heel spur is a hook of bone that forms on the calcaneus where the plantar fascia attaches. Heel spurs can be identified with an X-ray. A heel spur can occur with or without Plantar Fasciitis.
Causes
Though this syndrome is most common in individuals 40 years or older, it can occur at any age. The following factors increase the likelihood of heel spur development. An uneven gait which applies too much pressure to certain areas of the foot. Being overweight. Wearing worn shoes or ill-fitting footwear. Job conditions that require long periods spent standing or lifting heavy objects. The normal aging process which results in a decrease in ligament elasticity.

Symptoms
Most people think that a bone "spur" is sharp and produces pain by pressing on tissue, when in fact, these bony growths are usually smooth and flat. Although they rarely cause pain on their own, bone spurs in the feet can lead to callus formation as tissue builds up to provide added cushion over the area of stress. Over time, wear and tear on joints may cause these spurs to compress neighboring ligaments, tendons or nerves, thus injuring tissue and causing swelling, pain and tearing.
Diagnosis
Your doctor will discuss your medical history and will examine your foot and heel for any deformities and inflammation (swelling, redness, heat, pain). He/she will analyze your flexibility, stability, and gait (the way you walk). Occasionally an x-ray or blood tests (to rule out diseases or infections) may be requested.
Non Surgical Treatment
Acupuncture and acupressure can used to address the pain of heel spurs, in addition to using friction massage to help break up scar tissue and delay the onset of bony formations. Physical therapy may help relieve pain and improve movement. The Feldenkrais method could be especially helpful for retraining some of the compensation movements caused by the pain from the spur. Guided imagery or a light massage on the foot may help to relieve some of the pain. Other treatments include low-gear cycling, and pool running. Some chiropractors approve of moderate use of aspirin or ibuprofen, or other appropriate anti-inflammatory drugs. Chiropractic manipulation is not recommended, although chiropractors may offer custom-fitted shoe orthotics and other allopathic-type treatments.
Surgical Treatment
In a small number of cases (usually less than 5 percent), patients may not experience relief after trying the recommendations listed above. It is important that conservative treatments (such as those listed above) be performed for AT LEAST a year before considering surgery. Time is important in curing the pain from heel spurs, and insufficient treatment before surgery may subject you to potential complications from the procedure. If these treatments fail, your doctor may consider an operation to loosen the plantar fascia, called a plantar fascia release.
Prevention
There are heel spur prevention methods available in order to prevent the formation of a heel spur. First, proper footwear is imperative. Old shoes or those that do not fit properly fail to absorb pressure and provide the necessary support. Shoes should provide ample cushioning through the heel and the ball of the foot, while also supporting the arch. Wearing an orthotic shoe insert is one of the best ways to stretch the plantar fascia and prevent conditions such as heel spurs. Stretching the foot and calf is also helpful in preventing damage. Athletes in particular should make sure to stretch prior to any physical activity. Stretching helps prevent heel spurs by making tissue stronger as well as more flexible. In addition, easing into a new or increasingly difficult routine should be done to help avoid strain on the heel and surrounding tissue.